Infertility Treatment
Infertility Treatment in Nepal
Infertility is a serious health issue, affecting around 8-10% of couples, worldwide. Infertility treatments help couples to conceive a child when natural conception is not possible. Which treatment options to choose from depends on the underlying cause/s of infertility. After all the infertility diagnosis is done, your fertility specialist will work out your treatment plan and choose the best treatment available:
- Ovulation Induction: Ovulation Induction is a fertility treatment in which medicines are given to regulate ovulation. This is best suited to those who have irregular menstrual cycle. This is the first method that your doctors and fertility specialists at Vardhan will try to achieve your pregnancy goal. Before starting this treatment your doctor will thoroughly evaluate your case to find out any underlying causes of infertility, ensuring that the treatment option is best suited to you. Ovulation Induction involves the following steps:
Evaluation – the initial stage may include evaluation of blood tests to measure hormone levels; and ultrasound to see uterus and ovaries; and review your medical history and lifestyle choices
Stimulation – the medication given for this treatment stimulates the ovary for development of the follicles.
Monitoring – during this process your doctor will closely monitor you through regular ultrasound scan to see the number and size of developing follicles and the timing of ovulation.
Trigger injection – once the follicle reaches its optimal size, hormone injection (human chorionic gonadotropin – Hcg) will be administered to trigger ovulation.
Timed Intercourse or insemination – your specialist will then recommend the day of intercourse to maximize your chances of pregnancy.
Ovulation Induction is relatively a simple and non-invasive fertility treatment. However, it may carry some risks such as multiple pregnancies and ovarian hyperstimulation syndrome (OHSS). Unlike any other treatment this might also come with some risks, though. Our fertility specialists will always brief you on the benefits and potential risk of this treatment, and provide continuous monitoring throughout the treatment process.
- Artificial Insemination (IUI) – This is an invasive procedure in which washed and concentrated sperm is directly placed into a woman’s uterus. This is a good treatment option for those with ovulation concern, mild male infertility, unexplained infertility or when donor sperm or frozen sperm is being used. This treatment option can be used in conjunction with medication to increase the chances of conception. Following process is typically involved in this:
 Ovulation Monitoring: initially your menstrual cycle is monitored to determine the timing of ovulation by tracking hormone levels through blood tests and the development of ovarian follicles through ultrasound scans.
Ovulation Monitoring: initially your menstrual cycle is monitored to determine the timing of ovulation by tracking hormone levels through blood tests and the development of ovarian follicles through ultrasound scans.
Semen Processing: on the day of your IUI, semen sample is collected, washed and then the highest quality sperm is selected to obtain a better result.
Insemination Procedure: A thin catheter (tube) is inserted through the cervix into the uterus and the prepared sperm is directly placed in the uterus. The procedure takes a few minutes and is usually done without anesthesia. However, you might feel slight cramping but can carry on with your day-to-day routine after taking rest in the clinic for half an hour.
Pregnancy Testing: Approximately after 2 weeks you are recommended to undergo a pregnancy test, which is followed by a visit to your fertility specialist to discuss the test result and the future course of action.
IUI is generally considered a less invasive and less costly fertility treatment as compared to IVF. The success rate may depend on various factors, such as cause of infertility, woman’s age and the quality of sperm used. Like any other treatment this might also have its benefits and potential risks which will be explained to you by our fertility specialists before starting the treatment.
 In vitro fertilization (IVF)/TEST TUBE BABY – IVF is a form of assisted reproductive technology (ART) in which an egg is fertilized with sperm outside the body within a glass in laboratory. During this process eggs are retrieved from a woman’s ovaries, fertilized with sperm in a laboratory dish and then the fertilized eggs (embryo) is transferred back into the woman’s uterus. Not all patients will be recommended IVF treatment. The fertility treatment for you completely depends on the underlying cause of infertility. IVF is recommended under these conditions:
In vitro fertilization (IVF)/TEST TUBE BABY – IVF is a form of assisted reproductive technology (ART) in which an egg is fertilized with sperm outside the body within a glass in laboratory. During this process eggs are retrieved from a woman’s ovaries, fertilized with sperm in a laboratory dish and then the fertilized eggs (embryo) is transferred back into the woman’s uterus. Not all patients will be recommended IVF treatment. The fertility treatment for you completely depends on the underlying cause of infertility. IVF is recommended under these conditions:
- Low ovarian reserve.
- Blocked fallopian tubes.
- Diagnosed with endometriosis or PCOS (Polycystic Ovary Syndrome).
- Moderate to severe male factor infertility.
- Partners with unexplained infertility.
- Aged female.
- Recurring miscarriages.
- Other fertility treatments exhausted with no result.
- Preservation of fertility for medical reasons, such as, certain cancer treatment which might affect fertility.
IVF PROCESS:
Ovarian Stimulation – You will be given hormone therapy to stimulate the ovaries to produce more eggs than usual. These hormones are given in the form of injection (follicle stimulation hormone – FSH, and luteinizing hormone – LH) for 8-14 days.
Monitoring – At Vardhan Fertility Centre, our specialists will regularly monitor the development of follicles through blood tests and transvaginal ultrasound (TVS). This will help your fertility specialists to adjust the dosage of hormones as needed and determine the timing of egg retrieval.
Trigger injection – Once the follicles have reached the desired size, ovum pick-up (egg pick-up) day is scheduled. You will be then given a shot of trigger injection of Hcg (human chorionic gonadotropin) which will complete the maturation of eggs, followed by procedures to collect the egg after 34-36 hours.
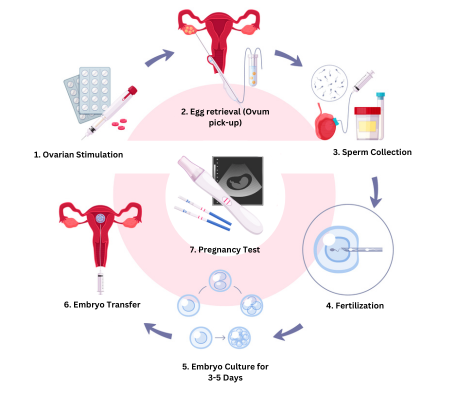
Egg retrieval (Ovum pick-up) – In this stage, matured eggs are collected from the ovaries. This is a day when surgery procedure is usually done under general anesthesia (IVA). Using ultrasound technology your fertility expert will locate the follicles in the ovaries and with the help of a thin needle s/he will collect the fluid and the eggs from the follicles. The procedure only takes 10-20 minutes.
Sperm collection – On the same day, sperm is collected from your partner and high quality sperm is prepared and selected for fertilization.
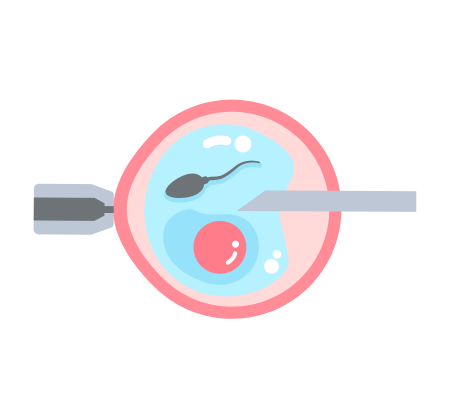
Fertilization – The eggs and sperm are then placed in a dish and then in a specialized incubator for fertilization. In some cases, single sperm is injected directly into each matured egg to facilitate fertilization. This specialized process is called intracytoplasmic sperm injection (ICSI). The embryologist will brief you on your embryo after 3 days of retrieval of your egg.
Embryo culture – The fertilized eggs (embryos) are cultured in the laboratory for around 3-5 days. During this time the embryologist will monitor the embryo for signs of healthy development.
Embryo transfer – One or more of the best quality embryos are transferred into the woman’s uterus. The number of embryos transferred depends on various factors, including the woman’s age, embryo quality, and previous IVF attempts. It is a simple day care procedure. It is performed using a thin catheter inserted through the cervix. Any additional embryos can be frozen and stored for potential future use.
Pregnancy test – You will be recommended for a pregnancy test approximately 12-14 days after your embryo transfer. If IVF is successful, the embryo implants in the uterine lining and pregnancy hormones (beta-Hcg) are detected in your blood test.
Whatever may be the result of pregnancy test, we will schedule an appointment to see your fertility specialist as soon as possible to plan further.
- Intracytoplasmic Sperm Injection (ICSI) – ICSI is a specialized procedure in IVF (in vitro fertilization) treatment where individual sperm is carefully injected directly into an egg (cytoplasm) by our experts. This process is usually best to treat severe male infertility issues such as low sperm count, low motility and severely morphologically defected sperms or even when there is a past history of a failed IVF procedure. ICSI is very similar to IVF process with key difference in the fertilization step in laboratory. In this process, semen sample is prepared in lab to separate as many healthy and most viable sperm as possible. And then our embryologist directly injects single sperm into each mature egg using a tiny needle under microscope, bypassing any natural barriers that may prevent fertilization. A typical ICSI process would include the following steps:
Ovulation stimulation: The woman undergoing the procedure typically receives hormone injections to stimulate her ovaries to produce multiple eggs.
Egg retrieval: Once the eggs reach a suitable size, they are retrieved from the woman's ovaries using a minor surgical procedure called follicular aspiration.
Sperm collection: On the same day as the egg retrieval, the male partner provides a sperm sample, which is processed to isolate the healthiest and most viable sperm.
Sperm injection: A single sperm is selected and injected into each mature egg using a specialized micromanipulation technique under a microscope.
Fertilization and embryo development: After the injection, the eggs are monitored to see if fertilization occurs. If successful, the fertilized eggs (embryos) are cultured in the laboratory for 3-5 days to allow them to develop.
Embryo transfer: Once the embryos reach a certain stage of development, one or more are selected for transfer into the woman's uterus. This is typically done 3 to 5 days after fertilization.
Pregnancy test: About 12 to 14 days after the embryo transfer, a pregnancy test is conducted to determine if the procedure was successful.
ICSI is often recommended when traditional IVF techniques have failed or there is severe male infertility factor present. It significantly improves the chances of fertilization for couples struggling with male factor infertility. However, it's important to note that ICSI doesn't guarantee pregnancy, and success rates can vary depending on various factors, including the quality of eggs and sperm, the expertise of the medical team, and the overall health of the individuals involved. It is always recommended that you discuss the options with your fertility experts. - Surgical Sperm Retrieval: Surgical Sperm Retrieval is a procedure used to collect sperm directly from the male reproductive tract for use in assisted reproductive techniques such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). SSR is typically performed in cases where the male partner is unable to ejaculate sperm naturally due to a blockage, injury, or other reproductive issues. There are several different techniques used for surgical sperm retrieval, depending on the specific circumstances of the individual:

Percutaneous Epididymal Sperm Aspiration (PESA): PESA involves the insertion of a fine needle directly into the epididymis, the tube where sperm are stored and matured outside the testicles. Sperm are aspirated (withdrawn) using a syringe attached to the needle.
Testicular Sperm Aspiration (TESA): TESA involves the insertion of a needle directly into the testicle to aspirate sperm from the testicular tissue. This technique is used when there is a blockage in the reproductive tract preventing sperm from reaching ejaculation.
Testicular Sperm Extraction (TESE): TESE is a surgical procedure that involves the removal of a small piece of testicular tissue through incision in the scrotum or the groin. The tissue is then examined under a microscope, and sperm are extracted from the seminiferous tubules within the testicle.
Microdissection Testicular Sperm Extraction (Micro-TESE): Micro-TESE is a specialized form of TESE using a high-powered microscope to identify and extract sperm-containing tissue from within the testicle. This technique is particularly useful for men with non-obstructive azoospermia, a condition where sperm production is impaired within the testicles.
After sperm retrieval, the collected samples are processed and prepared for use in assisted reproductive procedures such as IVF or ICSI. The specific technique used for sperm retrieval will depend on factors such as the underlying cause of male infertility, the quality and quantity of sperm needed or produced, and the expertise of the reproductive specialist performing the procedure. Surgical sperm retrieval can provide an option for couples facing male infertility issues to achieve pregnancy using assisted reproductive technologies. However, it is important to note that success rates can vary depending on factors such as the underlying causes of infertility and the quality of the retrieved sperm. Additionally, surgical sperm retrieval procedures carry risks such as bleeding, infection, and damage to surrounding tissues, so they should be performed by experienced and skilled reproductive specialists in a controlled medical environment



